AS embodied by the National Strategic Plan for Ending AIDS (2016 to 2030), the government has highlighted its intention to halt and reverse the AIDS (Acquired Immunodeficiency Syndrome) epidemic by 2030 on the back of meeting the 95-95-95 strategic targets or objectives – as the means to realise the country’s vision of securing the “Three Zeros”, i.e, zero new infections, zero discrimination and zero AIDS-related deaths.
These strategic targets or objectives aim for:
> 95% of the critical population to have their HIV status diagnosed and to be notified of the results;
> 95% of those who have HIV to be started on antiretroviral therapy (ART) treatment; and
> 95% of these (i.e, in reference to the 95% in the second bullet point – who have started the ART treatment) adhere to treatment with a suppressed/reduced viral load.
However, more has to be done to realise these envisioned goals.
It’s vital, therefore, for the government to ensure that the National Strategic Plan for Ending AIDS (2016 to 2030) and, by inclusion, the 95-95-95 strategic targets or objectives and, in turn, the “Three Zeros” are implemented holistically and comprehensively – entailing and necessitating a “whole of government, all society (private sector, civil society, communities and families)” approach.
To appreciate the overall situation, it’s important to re-highlight the nature of AIDS which is a condition resulting from HIV (human immunodeficiency virus) that is originated directly from sexual activities, principally via the exchange of bodily fluids, and is transmitted secondarily via the sharing of needles, exposure to infected blood, or passing on an infection from mother to child when pregnant (MTCT), which occurs during pregnancy, labour, delivery and breastfeeding.
The HIV virus attacks and destroys the immune system’s infection-fighting CD4 cells (CD4 T lymphocytes) that coordinate the immune response.
In other words, CD4 (white blood cells) play a significant role as a defence mechanism to fight against infections, viruses, etc.
The CD4 count for an average healthy person should range from 500 to 1500 cells per cubic millimetre of blood (mm3).
However, the number can decrease to 200 cells/mm3 and below in the case of a person with HIV whose condition has progressed or advanced to AIDS – which can vary (dependent variable) among individuals – e.g, as early as within six months or as late as 20 years in absence of ART.
The purpose of ART is to suppress the replication/multiplication of HIV (based on the formula of “undetectable equal untransmittable” – U=U – vis-à-vis the viral load).
Globally, about 38.4 million people were living with HIV in 2021 and 650,000 died in the same year alone.
As maintained by the Health Ministry (MOH), it is projected that 81,942 people were living with HIV (PLHIV) at the end of 2021 and 67,822 (83%) of these individuals were aware of their condition and were informed by the national surveillance system.
Whereas only 44,916 were receiving ART 0 which is only 55% of the total.
Normally, PLHIV are carriers – including those with AIDS – who continue living because of ART (i.e, longer than if they have not received ART).
However, ART for PLHIV increased to 66% last year compared with, for example, 28% in 2015.
However, according to Deputy Director-General of Health (Public Health) Datuk Dr Norhayati Rusli, “the declines in HIV cases and the increase in treatment coverage is still insufficient for the country to eliminate AIDS by 2030. Inequalities are the obstacle to this effort. Therefore, the availability, quality and suitability of services for HIV treatment, testing and prevention must be improved”.
There’s a critical need for an all-inclusive and comprehensive HIV treatment.
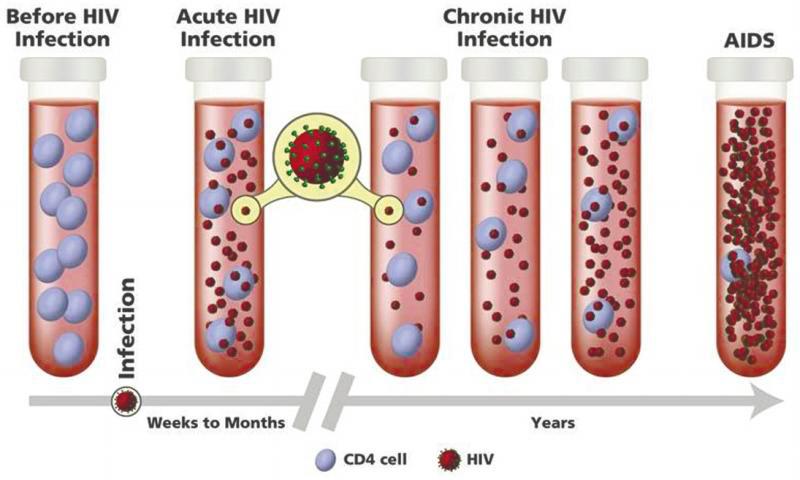
The US National Institute of Health has classified HIV into three main stages (Figure 1):
Stage 1: Acute HIV infection (seroconversion illness)
This is the initial stage of HIV infection which typically appears two to four weeks after HIV infection.
The risk of HIV transmission (i.e, from the carrier to another individual) significantly rises during the acute HIV infection stage due to the extremely high level of HIV in the blood.
Stage 2: Chronic HIV infection (asymptomatic /clinical latency)
The second stage is where the virus will continue to mutate at this stage albeit at very low levels and the CD4 count will continue to drop if proper treatment is not provided.
Stage 3: AIDS
Here, the CD4 count will hit less than 200 cells. The body cannot fight off opportunistic infections and infection-related cancers that occur more frequently or are more severe in people with weakened immune systems. Without ART, people with AIDS typically survive for about three years.
As reported in the Global AIDS Monitoring Report 2022 by MOH, infected patients are only aware of their condition in the later stages.
In 2021, 68% of infected patients with HIV were only diagnosed in the later stages due to a lack of awareness and concomitantly screenings/tests.
Beyond issues with late-stage diagnosis, PLHIV-related concerns in Malaysia also include:
->Stigmatisation and discrimination – household, workplace and society
Lack of political will to stem disinformation and fear-mongering has resulted in PLHIV being discriminated against and ostracised by family, the workplace and wider society. The welfare of the PLHIV community is also overlooked and neglected by politicians as policymakers.
Recently, the Selangor mufti department prohibited the administration of pre-exposure prophylaxis (PrEP) medication for homosexual couples in the state.
PrEP – a preventive medication for HIV transmission – is clinically proven to be able in preventing the spread of HIV by 99% during sex.
Notwithstanding, the absence of PrEP medication could increase the number of PLHIV and increase HIV transmission in the state.
->Inadequate coverage of health care services
As mentioned, only slightly more than half of the (reported) PHLIV community were receiving ART (in 2021).
The rest have not due to insufficient awareness, psychological barriers of the fear of stigmatisation (e.g, family members), financial constraints (especially when it comes to second-line treatment), etc.
Thailand, one of the few countries with the highest LGBTQ community, incorporated HIV services, including ART, into its universal health care scheme in 2006.
As a result of more than three-quarters of the 94% of the PLHIV who are aware of their status have achieved viral suppression, new infections in Thailand have decreased by two-thirds since 2010.
Additionally, since 2014, Thailand started providing ART to all PLHIV regardless of their CD4 count.
Malaysia should follow suit as well as part of the initiative to provide a holistic and comprehensive HIV treatment that’s inclusive and more equitable, thereby achieving the 95-95-95 strategic targets or objectives and “eliminating” the scourge of AIDS in the country and, thus, realising the ambition of the “Three Zeros”.
The following are the policy recommendations proposed by EMIR Research to the relevant stakeholders:
->Bolstering HIV early intervention programmes
MOH should bolster the current outreach programmes so that it is more inclusive and expansive – that is, the target should not be only primarily focused on those with a sexually active lifestyle and high-risk communities like sex workers, homosexuals (gays and lesbians), drug addicts, etc. But also the wider population inclusive of our migrant labour and the less developed regions too (e.g, Kelantan – the number of PLHIV due to homosexually-oriented transmission in the state has allegedly increased by 33.2% over the past five years).
The outreach programmes should have prevention as their aim alongside early intervention.
These include public awareness campaigns which should be run simultaneously with screenings for HIV.
At the same time, MOH should identify “hotspot” areas with a high number of HIV-positive people to provide integrated services for detection/screening, diagnosis, and advice/referral.
->Adding special provisions to the Prevention and Control of Infectious Diseases Act (1988)
The Prevention and Control of Infectious Diseases Act (1988) should be complemented and supplemented by special provisions about the achievement of the National Strategic Plan for Ending AIDS (2016 to 2030) together with the 95-95-95 strategic targets or objectives alongside the “Three Zeros”.
Towards that end, special regulations or subsidiary legislations should be prepared and implemented to ensure that PLHIV, who are yet to be detected or made aware of their condition report to screening and treatment, including tourists and visitors and our local foreign migrant labour population.
This could entail, making it compulsory for employers to periodically require their foreign workers to be subject to screening/testing and submit the results to the MOH, the Human Resources Ministry and Home Affairs Ministry.
->Providing psychological and nutritional services for PLHIV
Psychological and nutritional healthcare services are part of the broader HIV treatment regime.
It goes without saying that the mental health of an individual is significantly challenged and impacted by HIV.
This is in line with, for example, a study which found that almost one in every three people who suffer from a long-term physical medical condition also struggles with a mental health condition.
Not only that, having a wholesome, nutritious diet boosts general health and aids in immune system maintenance, which could play a vital role in complementing and supplementing the effects of ART.
In addition to having second-line ART and routine check-ups, PLHIV patients should be scheduled for a compulsory consultation session with a psychologist and nutritionist periodically.
Thus, PLHIV can be placed on a healthier lifestyle driven by a balanced and highly-nutritious diet alongside mental well-being.
->Providing State-supported health insurance policies for PLHIV
PLHIV are not insured with health insurance coverage in Malaysia as HIV does not fall under the category of critical illness.
This is due to the lack of awareness by insurance companies of the improvements in the long-term outlook for PLHIV.
Even where it’s available, the cost of these policies is high ranged whereby most middle-income and low-income PLHIV would not be able to afford them.
As such, the MySalam national health protection scheme should be expanded to include the first two stages of HIV infection.
Currently, this scheme only covers a) full-blown AIDS (CD4 count less than 200 cells) and also b) HIV infection due to blood transfusion.
In conclusion, while HIV is an incurable infection, the spread of this illness can be stopped, nevertheless, by intervening actions taken by the relevant stakeholders.
Jason Loh and Jachintha Joyce are part of the research team at EMIR Research, an independent think tank focused on strategic policy recommendations based on rigorous research. Comments: letters@thesundaily.com